疾患情報
大腸肛門機能科
Functional Anorectal Disorders
Takano Hospital Center for the Treatment of Functional Anorectal Disorders
|
Takano Hospital
Center for the Treatment of Functional Anorectal Disorders
Many people experience constipation, diarrhea, fecal incontinence, and difficult evacuation accompanied by a feeling of fullness and abdominal pain. These conditions often cause a decline in the quality of life (QOL).
Although the issue of incontinence is socially less recognized, the situation concerning many people who suffer from incontinence is as serious as the conditions facing people with colon and rectal cancer or other anal diseases.
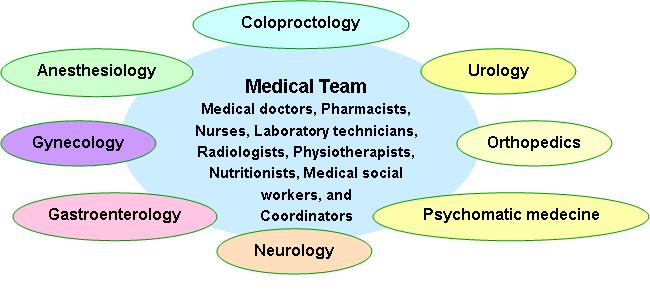
The international criteria of the Rome III classification, divides the Functional Anorectal Disorders into seven separate disorders (Table 1). However, we have combined these disorders into a single syndrome and named it, “Neurogenic Intrapelvic Syndrome” (NIS). We will provide appropriate treatment after consultation and a thorough examination.
If you have any problems related to Functional Anorectal Disorders please don’t hesitate to come and see us.
Table 1 Functional Anorectal Disorders
F. Functional anorectal disorders F1. Functional fecal incontinence
F2. Functional anorectal pain
F2a. Chronic proctalgia
F2a1. Levator ani syndrome
F2a2. Unspecified functional anorectal pain
F2b. Proctalgia fugax
F3. Functional defecation disorders
F3a. Dyssynergic defecation
F3b. Inadeequate defecatory propulsion
Bharucha AE, et al.: Functional Anorectal Disorders. Gastroenterology 2006:130:1510-1518
The following schedule outlines the days and times Takano Hospital receives patients who would like to consult with and be examined by one of our physicians:
To speed up the registration process please download and fill-out the questionnaire in the PDF file below before visiting the hospital.
Neurogenic Intrapelvic Syndrome (NIS) What is neurogenic intrapelvic syndrome (NIS)?
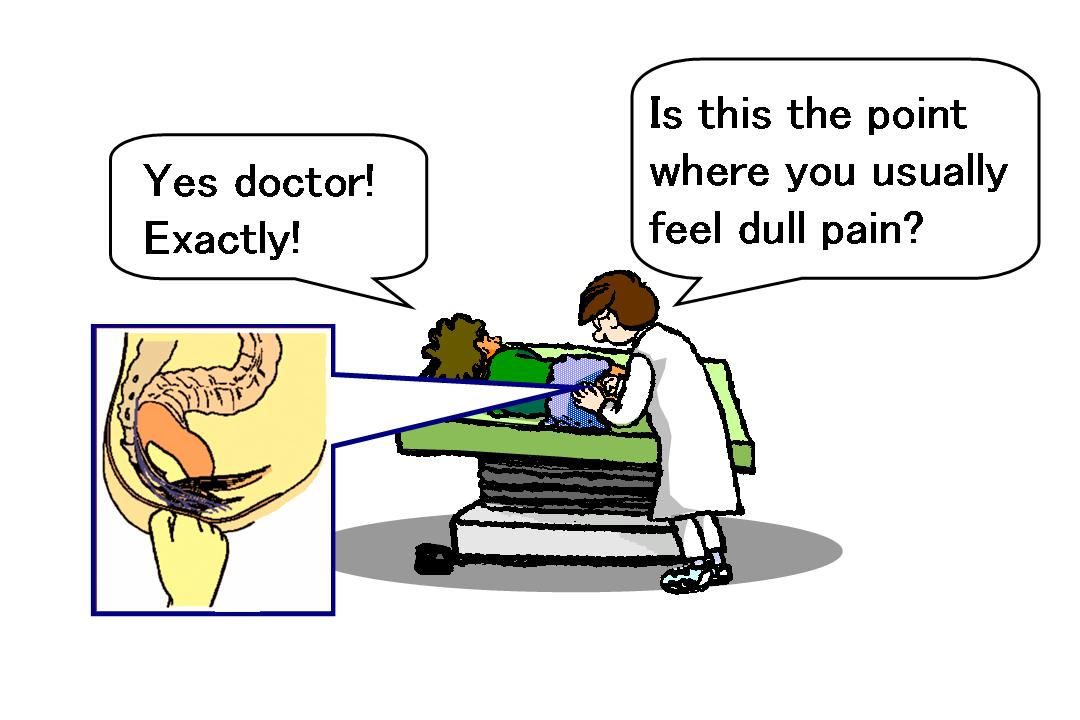 There are many patients who complain of chronic anal and pelvic pain that unfortunately, is mistakenly thought to originate from the sacrum, coccyx, ligament or muscle. Although the patients visited many clinics and hospitals, the ailment was not properly treated, and these patients suffered from the pain for long periods of time. However, when they were thoroughly examined, it was found that the origin of their pain was the tender indurations along their pudendal nerve. In addition to the pain, they often complain of constipation, incontinence of stool, flatus caused by dysfunctions of the anus, difficult evacuation and/or a feeling of incomplete evacuation caused by dysfunctions of the rectum, abdominal pain and a feeling of fullness due to fecal matter and gas build-up in the colon. We named the combination of these symptoms the “Neurogenic Intrapelvic Syndrome” (NIS) and we treat them as a single syndrome. One of the most common characteristics of NIS is the palpation of tender indurations along the pudendal nerve, which plays an important role in defecation and urination in conjunction with the intrapelvic splanchnic nerves. The pudendal nerve innervates the urethra and anus and the intrapelvic splanchnic nerves innervate the urinary bladder and rectum. In NIS, the above-mentioned complex combination of the 5 symptoms creates a syndrome that is caused by the disorders of the two nerves. The pain observed in NIS often intensifies and continues to the point where it may cause psychological problems.
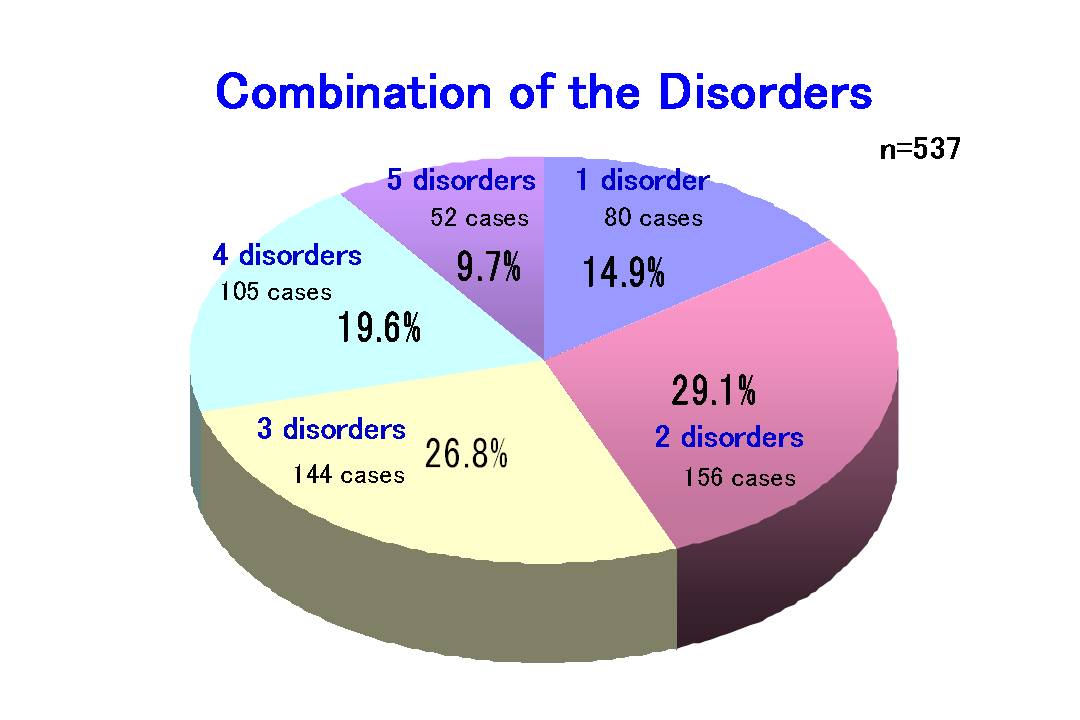
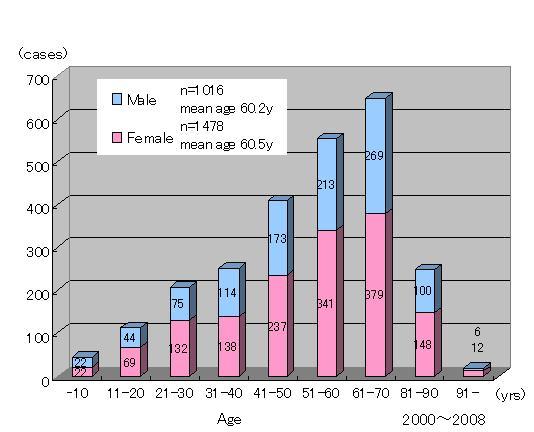 Age distribution Quite a few people come to our hospital complaining of symptoms related to NIS. The figure to the right shows a wide age distribution of both male and female patients, with the majority of them being elderly, who suffer from NIS. 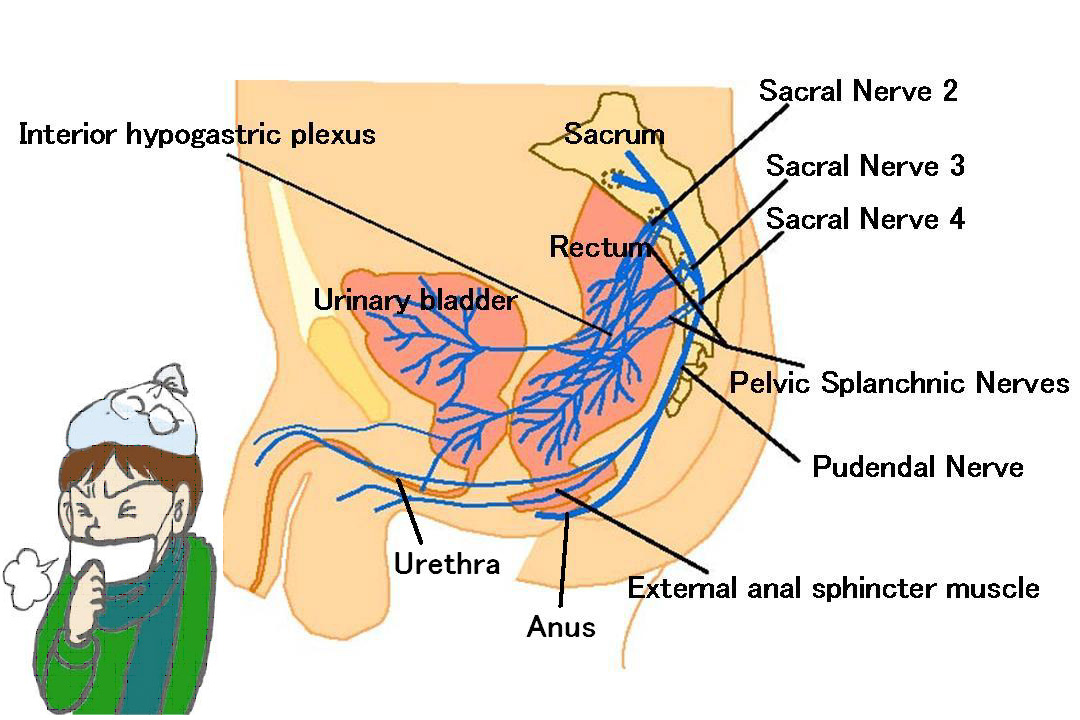 The 5 symptomatic groups of NIS Here, the 5 symptomatic groups of NIS are explained in more detail. In most of the NIS cases, the 5 groups of symptoms appear in various combinations. Moreover, NIS resembles the common cold which is usually accompanied by such symptoms as: sneezing, runny nose, coughing, fever, and headaches.
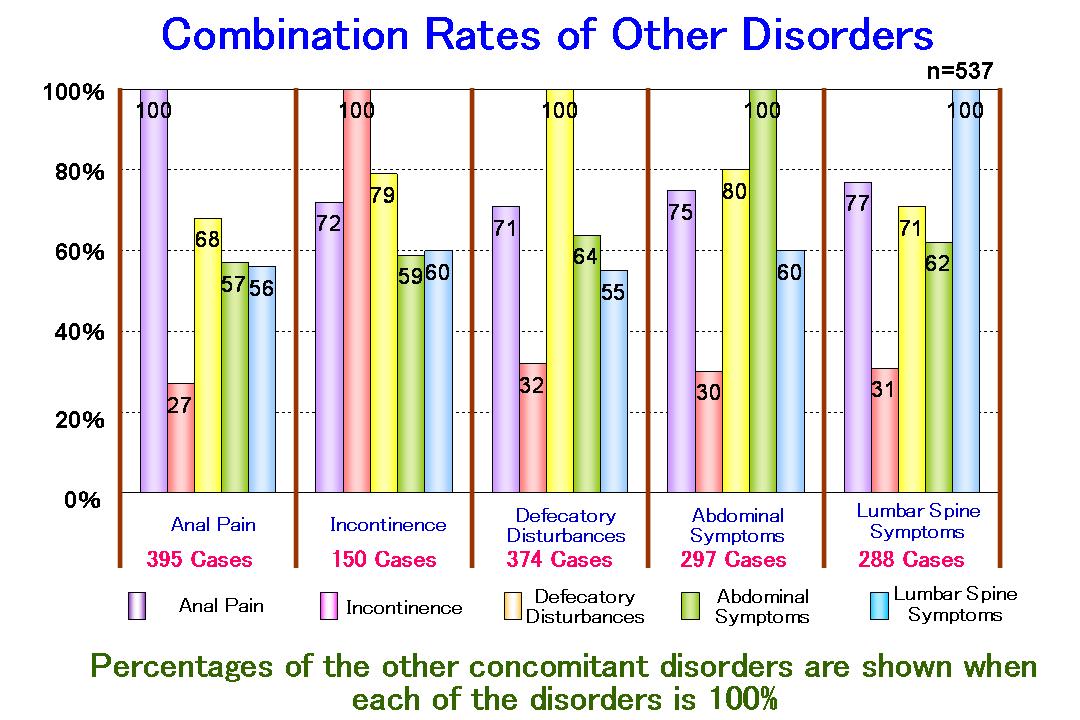
1. Anal pain
It is a dull pain that usually increases when patients sit for a long period of time. When examined, tender indurations are found along the pudendal nerve at the lateral sides of the sacrum. Digital compression of the nerve elicits the same kind of pain the patient usually experiences. 2. Incontinence Some patients complain of a leakage of stool and/or flatus. The function of the pudendal nerve is to control anal motility and anal sensation. The disturbance of this nerve will result in a lack of motility and sensation leading to incontinence of stool and flatus. On the other hand, In some cases, evacuation becomes difficult. 3. Defecatory disturbances Defecation is prompted by the motility and sensation of the anus and rectum. The pelvic nerve and the intrapelvic splanchnic nerves originating from the 2nd, 3rd and 4th sacrum trigger the sensation and motility of the rectum. When either or both of the nerves are damaged, the functions of the anus and/or the rectum are impaired resulting in difficult evacuation. 4. Abdominal symptoms Colonic functional disturbance usually results in abdominal pain and distention. When stool accumulates in the rectum by rectal and anal dysfunction, the colon becomes spastic in order to evacuate the stagnant stool. The result is that it becomes even more difficult to pass the stool through the spastic colon. The abdominal symptoms are somewhat similar to those of IBS. 5. Lumbar spine symptoms Lesions of the lumbosacral bones and/or cartilage disks result in lumbago and impairment of the sacral nerves. The syndrome appears with high combination rates with other symptoms.
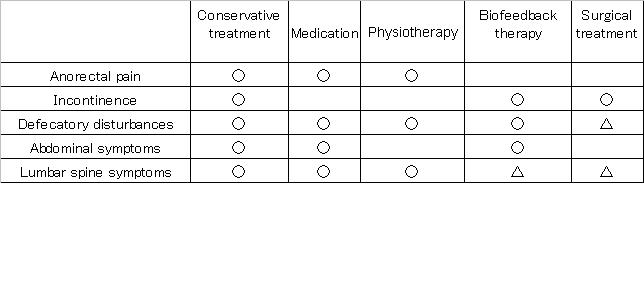
Patient History and examination Examinations Pharmacological treatment *Operational therapies Symptoms and Recommended Treatments
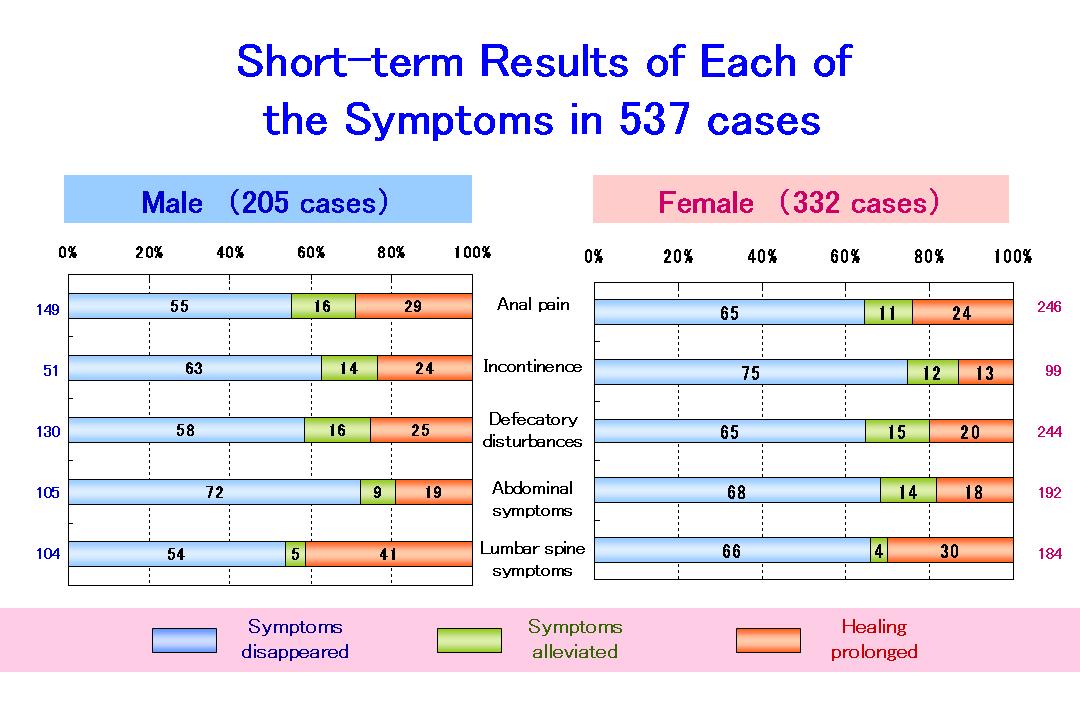
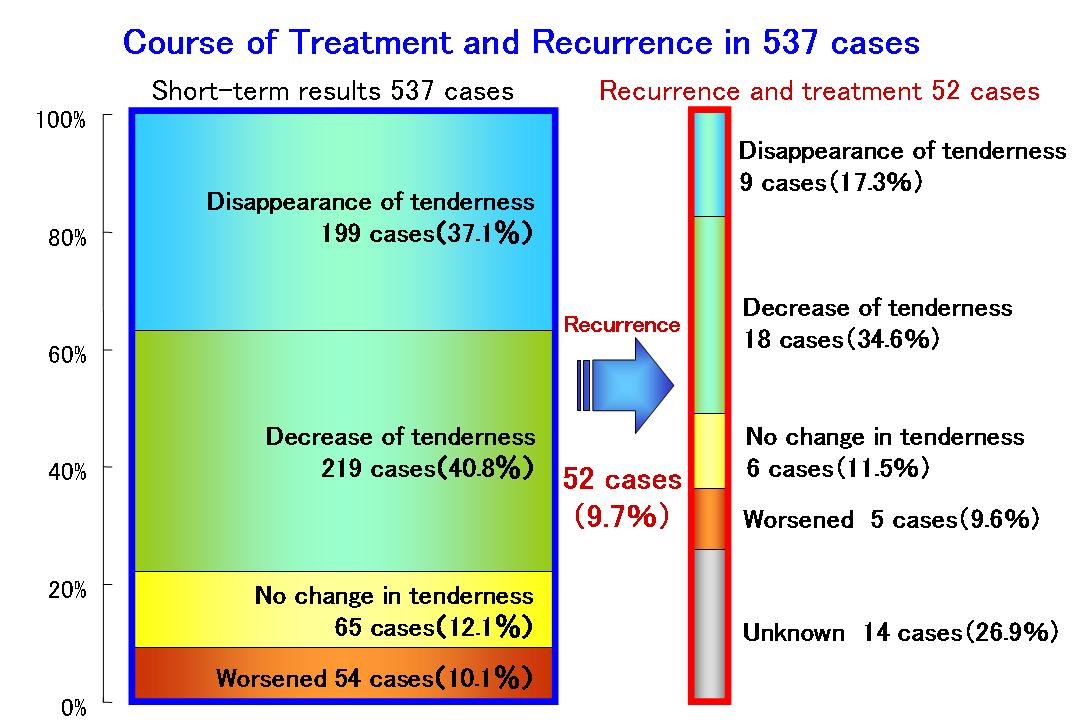
The results of the above-mentioned treatments over a five year period (2001-2005) are outlined below. When the 5 main symptoms are individually analyzed, 60-70% of the symptoms disappeared in both men and women within 9 months. When the number of patients who exhibit an improvement in their condition is added, the efficacy rate of the treatment is further increased to around 80%. Recurrence is one of the characteristics that tend to accompany this syndrome. For instance, about 10% of all the patients experience recurrence in the form of tenderness of the pudendal nerve. However, with further treatment, the tenderness in 50% of those cases disappears.
Masahiro TAKANO M.D.
|
|||||||||||||